Definition
Hallux valgus is the most common foot deformity.
It is a progressive foot deformity in which the first metatarsophalangeal (MTP) joint is affected and is often accompanied by significant functional disability and foot pain and reduced quality of life
This joint is gradually subluxed. There is medial deviation of the first metatarsophalangeal (MTP) joint and lateral deviation of the great toe. This results in abduction of the first metatarsal while the phalanges adduct
This often leads to the development of soft tissue and bony prominence on the medial side of what is called a bunion (exostosis on the dorsomedial aspect of the first metatarsal head).
At a late stage, these changes lead to pain and functional deficit: i.e. impaired gait (lateral and posterior weight shift, late heel rise, decreased single-limb balance, pronation deformity)
There is a high prevalence of hallux valgus in the overall population (23% of adults aged 18-65 years[10] and 35.7% of adults over 65 years of age)
There is a higher prevalence in women (females 30% - males 13%) and the elderly (35.7%)
It is more common in individuals with flat feet or hammer toes

The Hallux or first toe is the medio-distal part of the foot.
• Formed by the first metatarsal (articulates with two sesamoid bones), the first proximal phalanx and the first distal phalanx.
• Formed by three bones instead of four, unlike the other toes who have an extra bone called the intermediate phalanx.
The Hallux (first toe) has three synovial joints.
Two sesamoid bones articulate with the first metatarsal bone. These sesamoid bones:
• Protect the tendons of Flexor Hallucis Brevis FHB (embedded in the tendon of the FHB muscle)
• Main function helping FHB generate more force by extending its levers.
Muscles acting on joint:
M. tibialis anterior, M. extensor hallucis longus, M. peroneus longus, M. flexor hallucis longus, M.extensor Hallucis Brevis, M. abductor hallucis, M. flexor hallucis brevis, M. adductor hallucis, M. interossei dorsales I, aponeurosis plantaris.
Hallux Valgus Angle
• The angle created between the lines that longitudinally bisect the proximal phalanx and the first metatarsal
• Less than 15° is considered normal. Angles of 20° and greater are considered abnormal. An angle of 45-50° is considered severe.
Epidemiology and Aetiology
Aetiology is not well established - certain factors have been considered to play a role in the development of hallux valgus:
• Gender (more common in women than men
• Footwear (tight pointed shoes)
• A recent review by Colò et al. has found that while certain footwear might increase symptoms, "a direct correlation with the development of the condition has not been detected [...] In predisposed patients, incorrect footwear is more a way to increase symptoms than a real risk factor for the development of the disease.
• Congenital deformity or predisposition
• Chronic achilles tightness
• Severe flatfoot
• Hypermobility of the first metatarsocunieform joint
• Systemic disease
• Possible that abnormal muscle insertions are partly responsible for hallux valgus
• Hallux valgus is also associated with hip and knee OA and is inversely associated with a higher BMI.
Dysfunctions that may be present:
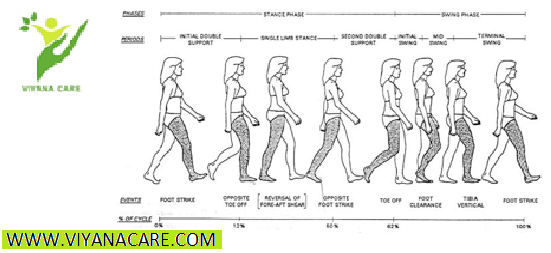
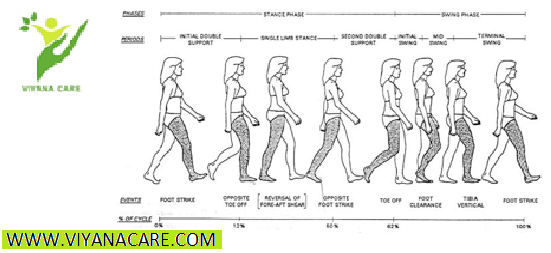
Gait deviations in the midstance (middle stage) and the propulsion phase (late stance). As the bodyweight moves forward on a foot on the ground, the patient will tend to keep his weight on the lateral border of the foot. This leads to a lateral and posterior weight shift
Patient has also a pronation deformity
The patient is unable to supinate his / her foot and will tend to keep his body weight on the lateral border of the foot which results in a late heel rise
The period of single-limb support will be diminished
When a physical examination is executed, the following indications could be present:
Lateral deviation of the MTP joint
Swelling of first MTP joint
Shortening of flexor hallucis brevis muscle
Tenderness of hallux
Weakness of hallux abductor muscles
Pain (primary symptom)
Diagnostic ProceduresManchester-Scale.png
Radiographs - used to determine the Hallux Valgus Angle (The angle created between the lines that longitudinally bisect the proximal phalanx and the first metatarsal)
Angle is greater than 15°, hallux valgus is diagnosed.
Angle of 45-50° is considered serious.
The degree of displacement of the sesamoids and the level of osteoarthritic change within the first MTP joint should be considered as well.
It is not always possible or necessary to take radiographs to determine the severity of hallux valgus. Therefore, the Manchester scale was developed .
The Manchester scale consists of standardized photographs of four types of hallux valgus: none, mild, moderate and severe. Research has shown that this scale is reliable in terms of both re-test and inter-tester reliability (kappa values of 0.77 and 0.86).
In the study by Roddy et al (2007) , the authors developed a tool that consists of five photographs instead of four. Each photograph had a hallux valgus angle increased with 15°. This tool had a good retest reliability (kappa = 0.82) and is also a good tool to use to determine hallux valgus severity . Both scales (the four-level classification or dichotomised scale) can be used to determine the severity of hallux valgus.
Physical examination should be performed with the patient both seated and standing. Take note of:
Deformity during weight bearing (generally accentuated).
Presence of pes planus and/or contracture of the Achilles tendon
Height of the longitudinal arch and hallux, with its relation to the lesser toes .
Differential Diagnosis
Hallux valgus can be confused with other diseases or injuries during diagnosis. In the early stages, the redness and pain can be confused with an inflammation, infection or gout of the first MTP joint.
Gout Pain suddenly appears while onset is gradual with hallux valgus. As well, semi uric acid level can be tested to differentiate between the two (since it is increased in patients with gout).
Hallux Rigidus can be confused with hallux valgus
Septic arthritis i(red and swollen).
Turf toe can be confused with hallux valgus.
Non-operative treatmentHallux valgus
Prevention
A hereditary factor or predisposition (for example as a result of a generalized ligamentous laxity) is not preventable but other things are. For example, wearing shoes that fit properly (not too tight) and avoiding high heels can be important factors in preventing hallux valgus.
Treatment
The first treatment option is non-operative care:
Adjustment of footwear to help in eliminating friction at the level of the medial eminence (bunion) e.g., patients should be provided of a shoe with a wider and deeper toe box
The condition of pes planus may be helped by an orthosis. Severe pes planus can lead to a recurrence of hallux valgus following surgery.
Achilles tendon contracture may require stretching or even lengthening .
This type of treatment can be applied in the early stage when the secondary contractures of the soft tissues and the alterations of the articular surfaces have not become permanent .
Operative treatment
If non-operative treatment fails, surgery could be considered . Before an operation is chosen, the severity of the hallux valgus has to be determined. In order to do that, a weight bearing plain film radiography is used.
Hallux valgus is the most common foot deformity.
It is a progressive foot deformity in which the first metatarsophalangeal (MTP) joint is affected and is often accompanied by significant functional disability and foot pain and reduced quality of life
This joint is gradually subluxed. There is medial deviation of the first metatarsophalangeal (MTP) joint and lateral deviation of the great toe. This results in abduction of the first metatarsal while the phalanges adduct
This often leads to the development of soft tissue and bony prominence on the medial side of what is called a bunion (exostosis on the dorsomedial aspect of the first metatarsal head).
At a late stage, these changes lead to pain and functional deficit: i.e. impaired gait (lateral and posterior weight shift, late heel rise, decreased single-limb balance, pronation deformity)
There is a high prevalence of hallux valgus in the overall population (23% of adults aged 18-65 years[10] and 35.7% of adults over 65 years of age)
There is a higher prevalence in women (females 30% - males 13%) and the elderly (35.7%)
It is more common in individuals with flat feet or hammer toes

The Hallux or first toe is the medio-distal part of the foot.
• Formed by the first metatarsal (articulates with two sesamoid bones), the first proximal phalanx and the first distal phalanx.
• Formed by three bones instead of four, unlike the other toes who have an extra bone called the intermediate phalanx.
The Hallux (first toe) has three synovial joints.
Two sesamoid bones articulate with the first metatarsal bone. These sesamoid bones:
• Protect the tendons of Flexor Hallucis Brevis FHB (embedded in the tendon of the FHB muscle)
• Main function helping FHB generate more force by extending its levers.
Muscles acting on joint:
M. tibialis anterior, M. extensor hallucis longus, M. peroneus longus, M. flexor hallucis longus, M.extensor Hallucis Brevis, M. abductor hallucis, M. flexor hallucis brevis, M. adductor hallucis, M. interossei dorsales I, aponeurosis plantaris.
Hallux Valgus Angle
• The angle created between the lines that longitudinally bisect the proximal phalanx and the first metatarsal
• Less than 15° is considered normal. Angles of 20° and greater are considered abnormal. An angle of 45-50° is considered severe.
Epidemiology and Aetiology
Aetiology is not well established - certain factors have been considered to play a role in the development of hallux valgus:
• Gender (more common in women than men
• Footwear (tight pointed shoes)
• A recent review by Colò et al. has found that while certain footwear might increase symptoms, "a direct correlation with the development of the condition has not been detected [...] In predisposed patients, incorrect footwear is more a way to increase symptoms than a real risk factor for the development of the disease.
• Congenital deformity or predisposition
• Chronic achilles tightness
• Severe flatfoot
• Hypermobility of the first metatarsocunieform joint
• Systemic disease
• Possible that abnormal muscle insertions are partly responsible for hallux valgus
• Hallux valgus is also associated with hip and knee OA and is inversely associated with a higher BMI.
Dysfunctions that may be present:
Gait deviations in the midstance (middle stage) and the propulsion phase (late stance). As the bodyweight moves forward on a foot on the ground, the patient will tend to keep his weight on the lateral border of the foot. This leads to a lateral and posterior weight shift
Patient has also a pronation deformity
The patient is unable to supinate his / her foot and will tend to keep his body weight on the lateral border of the foot which results in a late heel rise
The period of single-limb support will be diminished
When a physical examination is executed, the following indications could be present:
Lateral deviation of the MTP joint
Swelling of first MTP joint
Shortening of flexor hallucis brevis muscle
Tenderness of hallux
Weakness of hallux abductor muscles
Pain (primary symptom)
Diagnostic ProceduresManchester-Scale.png
Radiographs - used to determine the Hallux Valgus Angle (The angle created between the lines that longitudinally bisect the proximal phalanx and the first metatarsal)
Angle is greater than 15°, hallux valgus is diagnosed.
Angle of 45-50° is considered serious.
The degree of displacement of the sesamoids and the level of osteoarthritic change within the first MTP joint should be considered as well.
It is not always possible or necessary to take radiographs to determine the severity of hallux valgus. Therefore, the Manchester scale was developed .
The Manchester scale consists of standardized photographs of four types of hallux valgus: none, mild, moderate and severe. Research has shown that this scale is reliable in terms of both re-test and inter-tester reliability (kappa values of 0.77 and 0.86).
In the study by Roddy et al (2007) , the authors developed a tool that consists of five photographs instead of four. Each photograph had a hallux valgus angle increased with 15°. This tool had a good retest reliability (kappa = 0.82) and is also a good tool to use to determine hallux valgus severity . Both scales (the four-level classification or dichotomised scale) can be used to determine the severity of hallux valgus.
Physical examination should be performed with the patient both seated and standing. Take note of:
Deformity during weight bearing (generally accentuated).
Presence of pes planus and/or contracture of the Achilles tendon
Height of the longitudinal arch and hallux, with its relation to the lesser toes .
Differential Diagnosis
Hallux valgus can be confused with other diseases or injuries during diagnosis. In the early stages, the redness and pain can be confused with an inflammation, infection or gout of the first MTP joint.
Gout Pain suddenly appears while onset is gradual with hallux valgus. As well, semi uric acid level can be tested to differentiate between the two (since it is increased in patients with gout).
Hallux Rigidus can be confused with hallux valgus
Septic arthritis i(red and swollen).
Turf toe can be confused with hallux valgus.
Non-operative treatmentHallux valgus
Prevention
A hereditary factor or predisposition (for example as a result of a generalized ligamentous laxity) is not preventable but other things are. For example, wearing shoes that fit properly (not too tight) and avoiding high heels can be important factors in preventing hallux valgus.
Treatment
The first treatment option is non-operative care:
Adjustment of footwear to help in eliminating friction at the level of the medial eminence (bunion) e.g., patients should be provided of a shoe with a wider and deeper toe box
The condition of pes planus may be helped by an orthosis. Severe pes planus can lead to a recurrence of hallux valgus following surgery.
Achilles tendon contracture may require stretching or even lengthening .
This type of treatment can be applied in the early stage when the secondary contractures of the soft tissues and the alterations of the articular surfaces have not become permanent .
Operative treatment
If non-operative treatment fails, surgery could be considered . Before an operation is chosen, the severity of the hallux valgus has to be determined. In order to do that, a weight bearing plain film radiography is used.
